
How the disease develops
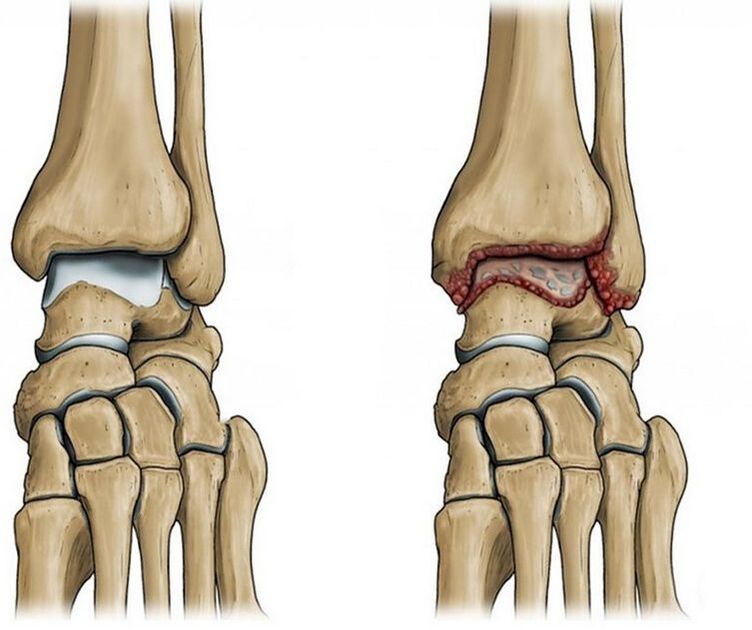
However, due to joint injury or natural aging, the joint surface becomes rough and the cartilage tissue loses smoothness and elasticity. When cartilage is damaged and degenerative changes progress, the bones begin to contact each other as they move within the joint, causing pain.
In an attempt to "defend" to compensate for further damage to the joint and surrounding tissue, osteophytes form - growths along the edges of the articular surfaces of bones. As a result, the joint's mobility is partially or even completely limited.
- Primary or idiopathic osteoarthritis. In this case, we are talking about degenerative dystrophic changes in the joints
- Secondary is related to exposure to a specific causative agent, usually a previous joint injury. This form is most commonly diagnosed
Predisposing factors
- Intra- and periarticular injuries, such as fractures, tears, and ligament ruptures
- ankle surgery
- Past inflammatory joint disease
- High-intensity loads: professional sports, ballet, long walks, work involving long periods of "standing"
- sedentary lifestyle
- Wearing high heels for a long time
- excess weight
- Inherited collagenopathies leading to impaired collagen synthesis
- Overloading causes chronic damage to joint structures
- Metabolic disorders: diabetes, gout
- Estrogen deficiency in postmenopausal women
- rheumatic diseases
- Foot deformities, such as flat feet
- Degenerative dystrophic changes in the spine, complicated by the formation of intervertebral hernias, accompanied by nerve root compression
Ankle Arthritis: Symptoms
Depending on the stage of pathological changes in the joint, the pain becomes more severe and persists at rest or even at night. Other symptoms occur.
- The first stage is characterized by mild swelling and redness of the skin around the joint, and pain in the afternoon or after strenuous exercise. The unpleasant sensation is concentrated on the front surface of the foot, the joint line and moves to the lateral surface of the ankle. X-rays of the feet may not show any changes yet.
- In the second stage, the pain becomes constant, there is a crunching sound when moving the joint, movement is limited, and the joint becomes "stuck. "Growths along the edges of the joint surfaces of bones are evident on X-ray: tibia, ankle, and talus, as well as narrowing of the joint spaces
- In the third stage, the joints deform, which is why only rocking, low-amplitude movements are possible. X-rays show massive bone hyperplasia and joint spaces that narrow or even disappear. Due to joint instability, patients often twist their legs, leading to sprains, torn ligaments, and worsening of general conditions, aggravating the condition.
- The maximum value expressed at the beginning of exercise - the so-called onset pain
- As the load increases significantly, especially when running and jumping
- Often appears in the evening, middle of the night or just after waking up
Symptoms appear in waves: exacerbations alternate with remissions. As the condition worsens, the symptoms become more obvious. During remission, symptoms gradually subside and may even disappear completely.
Which doctor should I contact?
diagnosis
- X-rays of the ankle joint are vital in diagnosing and determining the stage of the disease. Images show joint space narrowing, osteophytes at the edges of the articular surfaces of the bones, cysts, and signs of thinning of the bone beneath the cartilage
- CT scans of joints can provide a more detailed picture. Doctors can evaluate the condition of the patient's bone structure and cartilage tissue in detail
- MRI is used to study cartilage and soft tissue
- Joint Ultrasound to Evaluate the Structural Condition of Soft Joints
Treatment of Arthropathy
Correct lifestyle and nutrition
medical treatement
- Painkillers. Most commonly available as tablets, gels, or injections, NSAIDs are used to relieve pain and inflammation
- Antidepressants and anticonvulsants treat long-term, severe, difficult-to-treat pain
exercise therapy
massage
Auxiliary equipment
Surgery
Why are ankle joints dangerous?
As arthrosis progresses, the joints will become significantly deformed. Range of motion is drastically reduced, so the ability to support the foot becomes difficult; walking without crutches or a cane is almost impossible.
Chronic ongoing pain in joints can lead to anxiety and depression.
prevention
- Avoid traumatic activities. For example, jumping from high places, running
- avoid injury
- Be careful when it's icy and wear non-slip shoes
- Weight control
- Normalizing your weight will help reduce pressure on your ankle joints
- stay moderately active
- An inactive lifestyle is dangerous and can lead to complications, excessive overload, and microtrauma
- Keep your joints healthy
- Seek medical attention promptly and treat musculoskeletal disorders
- The prevalence of degenerative dystrophic diseases of the foot joints is 87%
- Occupational hazards, daily habits, and past injuries can all contribute to ankle arthritis.
- Common symptoms of joint disease - pain, crunching when moving, localized swelling, and subsequent restriction of foot movement
- Treatment of the ankle joint is usually conservative and includes both pharmacological and non-pharmacological methods.
- Progression of the ankle leading to disability and complete loss of foot function























